How functional medicine assessment can be a path to lasting recovery

Steve Bower // Shutterstock
How functional medicine assessment can be a path to lasting recovery
Traditional addiction treatment often focuses on managing symptoms through standardized protocols, typically centered on behavioral therapy, medication or a 12-step program. While these methods can be effective for some, they frequently overlook the unique biological, psychological and environmental factors that contribute to substance use disorders. As a result, relapse rates remain high, and many individuals struggle to hold on to long-term recovery.
By identifying underlying contributors, functional medicine in addiction recovery creates tailored strategies that support both body and brain healing. This method empowers people to understand their health better, make informed decisions and build a more stable foundation for sustained recovery. In doing so, it addresses addiction symptoms and the reasons behind them — offering a more straightforward path toward lasting well-being.
In this guide from The Sanctuary at Sedona, you’ll learn more about the process of functional medicine and how it can aid in addiction recovery.
Unveiling the Power of Functional Medicine: A New Approach to Addiction
Functional medicine is a patient-centered, science-based approach to addiction. Rather than treating addiction as a stand-alone diagnosis, it explores how various systems in the body interact and how imbalances may influence behavior and cravings. This shift in perspective is essential, especially for people whose substance use comes from chronic stress, inflammation, hormonal imbalances, unresolved trauma or nutritional deficiencies. A functional medicine assessment’s goals include:
- Identifying root causes: Functional medicine starts by determining underlying physiological, psychological and environmental factors contributing to substance use.
- Restoring systemic balance: Functional medicine aims to support the body’s interconnected systems, such as the immune response and detoxification pathways, to promote healing.
- Enhancing resilience: By restoring systemic balances, functional medicine improves stress response, emotional regulation and physical health to reduce the risk of relapse.
- Supporting long-term recovery: Functional medicine empowers people with sustainable tools and education to maintain their sobriety while improving overall well-being.
How Functional Medicine Differs From Traditional Addiction Treatment
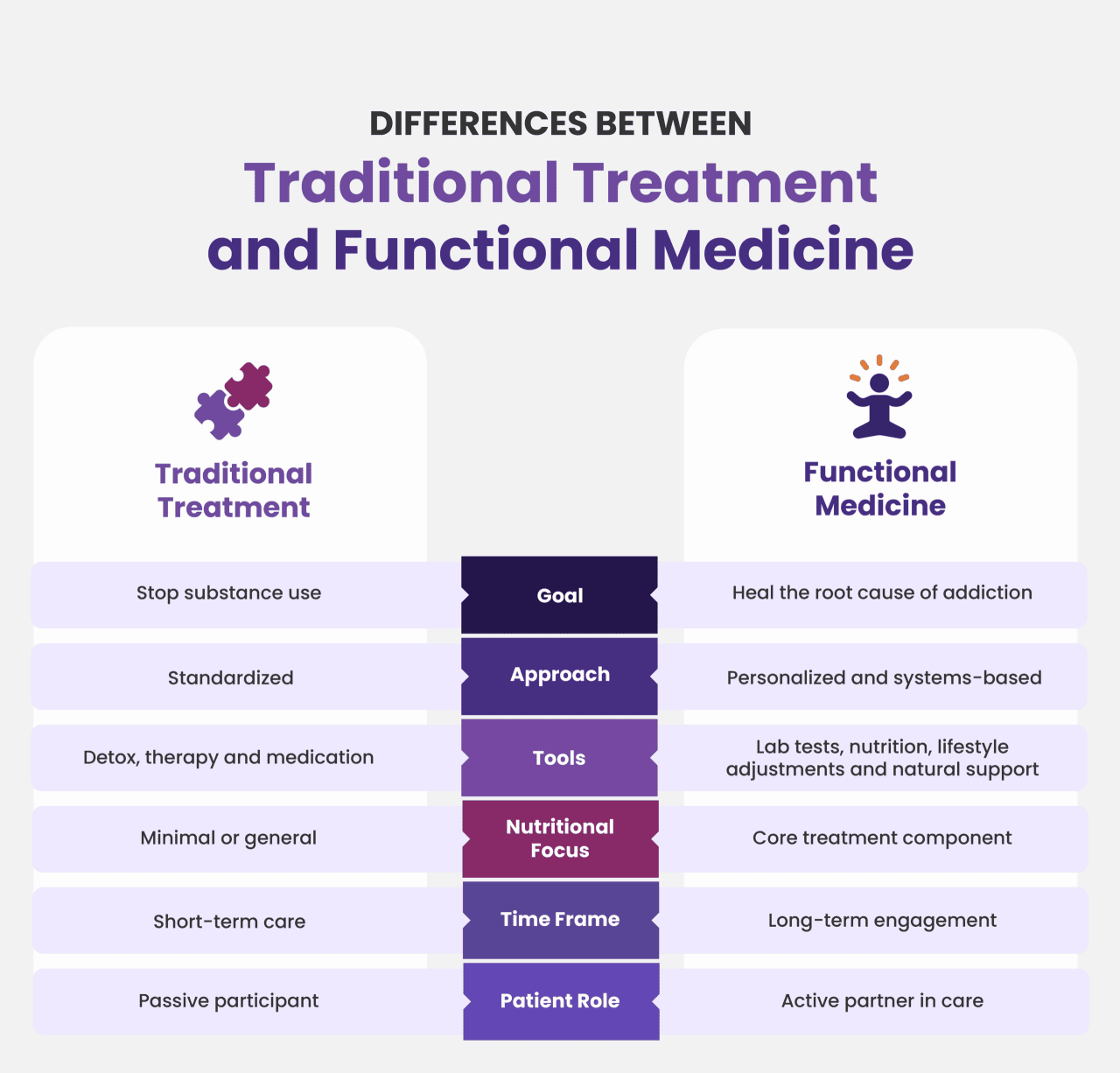
Traditional addiction treatment uses standardized protocols like detox, behavioral therapy and medication. It often treats addiction as a brain disorder or behavioral issue without exploring broader psychological factors. This means patients get a one-size-fits-all model, which may not account for individual variability in genetics, biology or life experiences.
Although functional medicine does not always align with standard short-term or emergency care protocols, it is science-based. This treatment differs in its approach, tools and treatment goals. It investigates underlying causes, which can include everything from gut dysfunction to chronic stress. This treatment recognizes addiction as a systemic issue influenced by multiple body systems and environmental inputs to create treatment plans based on the individual’s health history, lab results and life cycle.
Here’s a clearer breakdown of the distinctions between traditional addiction treatment and functional medicine:
The Sanctuary at Sedona
Why Functional Medicine Matters for Addiction
Recovery can start with traditional addiction treatment, but this treatment can fall short in preventing relapse and addressing the complexity of addiction. Many programs focus on behavioral strategies and medication management without exploring the broader biological and environmental context of substance use.
Functional medicine fills these gaps by using a systems-based approach to uncover what’s driving addictive behaviors on a deeper level. Instead of only focusing on symptoms like cravings or mood swings, the goal is to understand why these symptoms occur in the first place.
How Functional Medicine Identifies Root Causes
Functional medicine practitioners use detailed health histories, lifestyle evaluations and advanced laboratory testing. This information can reveal factors that may fuel compulsive behavior or emotional dysregulation. These factors include:
- Chronic inflammation
- Neurotransmitter imbalances
- Blood sugar instability
- Unresolved infections
- Nutrient deficiencies
- Mitochondrial dysfunction
- Environmental toxin exposure
Withdrawal is a challenging part of addiction recovery, encompassing the physical and psychological symptoms that occur when someone stops using an addictive substance. As the body struggles to function normally without these substances, patients experience increased anxiety, insomnia, nausea, agitation and other symptoms. Managing this stage correctly can stop relapse, and this management benefits greatly from functional medicine.
By targeting underlying addiction causes, functional medicine helps stabilize the body and the mind. Patients can expect improved mental clarity, fewer cravings, better sleep and stronger emotional resilience. These benefits support long-term recovery by restoring balance to systems that become damaged by substance abuse.
Addressing Co-Occurring Conditions
Holistic or functional treatments address co-occurring conditions. Substance use often coexists with mental health conditions like anxiety, depression, attention-deficit/hyperactivity disorder (ADHD) or post-traumatic stress disorder (PTSD). These conditions can stem from biochemical contributors, such as thyroid or adrenal dysfunction or neurotransmitter imbalances.
Improving Nutrition and Gut Health
Cravings can result from emotional, physical or environmental triggers during recovery. They often have biological roots in the brain’s reward circuitry, especially in the dopamine system. Common triggers include low blood sugar and nutrient deficiencies. Functional medicine focuses on restoring gut-brain balance by eliminating inflammatory foods, reintroducing nutrient-dense diets and rebuilding the intestinal barrier function, or leaky gut.
Reducing Inflammation and Oxidative Stress
Substance use can increase systemic inflammation and oxidative stress, which can damage the brain and body. Functional medicine uses targeted interventions like antioxidants, omega-3 fatty acids, mitochondrial support supplements and anti-inflammatory diets. These reduce inflammation, repair tissue damage and support cognitive function, which is critical for emotional stability during recovery.
Providing Holistic Support for Long-Term Sobriety
Functional medicine combines medical care with lifestyle coaching, offering physical activity programs, community and social support resources and stress management techniques. These components enhance emotional well-being and reduce relapse risk. They also align with the principles of biopsychosocial recovery models, which research consistently shows are effective.

The Sanctuary at Sedona
What to Expect During Your Functional Medicine Evaluation
A functional medicine assessment integrates multiple data points to develop a tailored treatment plan that supports the person, not only the addiction. During the assessment, you can expect:
- A detailed history review: Patients share a thorough timeline of health events, family history, past illnesses, medications and substance use patterns. This helps identify long-term imbalances and early warning signs easily missed in traditional assessments.
- A physical exam: The physical exam evaluates the individual’s current symptoms, physical health status and signs of systemic imbalances, such as fatigue or malnutrition.
- Laboratory testing: Functional labs are targeted and in-depth, testing for nutrient levels, various hormone panels, including cortisol, thyroid and adrenal function, and gut health markers that can affect mood or cravings.
- A psychological assessment: The psychological assessment reviews emotional trauma, coping patterns, mental health history and current mood disorders. Functional medicine practitioners examine how brain chemistry and emotional triggers relate to substance use.
- A lifestyle assessment: The lifestyle assessment explores sleep quality, diet, physical activity, stress levels and social support systems. It identifies habits that may either support or undermine recovery.
Each element of the assessment adds to a comprehensive understanding of the individual’s health. For example, a nutrient deficiency may explain fatigue, a gut dysfunction can indicate poor neurotransmitter production, and chronic sleep disruption might point to cortisol dysregulation. By connecting these factors, functional medicine practitioners identify hidden addiction drivers. Then, they can design a treatment plan that targets those imbalances, supporting sobriety and long-term wellness.
From Assessment to Action: Crafting Your Personalized Recovery Plan
Functional medicine enhances traditional addiction treatment by offering an insightful view of each person’s health and recovery needs. By integrating information from lab testing, medical history, psychological evaluation and lifestyle analysis, practitioners create a targeted approach that addresses the specific environmental and biological factors contributing to substance use:
- Root cause mapping: Assessment data is organized into interconnected systems, such as the digestive, endocrine, immune and nervous systems, to identify where there are imbalances or dysfunctions. This mapping highlights the main drivers for addiction-related symptoms.
- Personalized prioritization: Functional medicine does not treat all issues at once. Practitioners prioritize interventions based on severity, symptom burden and patient readiness. For example, severe gut inflammation or blood sugar instability may be treated before hormone support. Nutrient replacement may also be treated before cognitive-behavioral interventions when deficiencies are impairing brain function.
- Data-driven goal setting: Objective markers like cortisol levels or inflammatory markers help define short- and long-term treatment goals. Progress is tracked using repeat labs and symptom questionnaires.
Based on assessment findings, a variety of integrative treatment options can be combined to restore health and support lasting recovery. The goal is to create individualized relapse shields to protect individuals from returning to substance use after the initial sobriety. These proactive strategies strengthen the body and mind against stress, temptation and emotional setbacks.
Nutritional Therapy
Diet plays a keen role in addiction recovery and mental health. Optimal brain function and regulation need adequate protein, vitamins and minerals. Too much of the wrong nutrients, such as a diet of processed carbohydrates, increases blood pressure and can fuel conditions like depression.
Nutritional therapy rebuilds biochemical balance and repairs damage from substance use. Individual diets are based on food sensitivities, lab results and metabolic needs. For example, a client with hypoglycemia may be put on a high-protein, low-glycemic meal plan to stabilize blood sugar and reduce cravings.
Supplementation
The purpose of supplementation is to correct nutrient deficiencies and support detoxification, brain health and energy production. Supplement prescriptions are based on individual tolerance and lab values, including:
- B vitamins for neurotransmitter synthesis.
- Magnesium for calming the nervous system.
- Omega-3 fatty acids to reduce inflammation and improve mood.
- Adaptogens to support adrenal health and resilience.
Lifestyle Interventions
High-quality sleep can reduce stress, alleviate brain fatigue and promote healthy brain function. In the same way, exercise and physical activity release endorphins, boosting mood while lowering stress levels. When the brain and body function optimally, patients can focus on their long-term recovery.
Lifestyle interventions establish routines that support mental, physical and emotional healing. These include stress management practices, sleep hygiene plans for restoring circadian rhythm and exercise regimens tailored to current fitness and adrenal health. They often include coaching or group education to encourage sustainable change.
Complementary Therapies
To support the mind-body connection and enhance nervous system regulation, practitioners recommend complementary therapies. Acupuncture reduces anxiety and depression, massage therapy improves detox, and mindfulness-based practices like meditation build emotional resilience. When used with other approaches, mindfulness-based therapies can also reduce cravings and the risk of relapse.
People in recovery can also boost their healing process by using biotechnology and tools. Smartphone apps and smartwatches with health-monitoring features, such as activity levels, heart rate and blood pressure, help those in recovery track how complementary therapies and lifestyle interventions impact their physical health. Some facilities offer more innovative biohacking treatments, including:
- Dry flotation
- Colon hydrotherapy
- Infrared sauna
In rare cases, medications are used to stabilize acute symptoms and support early recovery stages. Their use is selective, often along with natural therapies, with frequent reevaluation as healing progresses. These medications can include buprenorphine for a broader recovery plan or selective serotonin reuptake inhibitors (SSRIs) for severe depression alongside nutritional and gut interventions.
Reclaim Your Life: The Transformative Nature of Functional Medicine
The benefits of functional medicine go beyond sobriety. This approach offers patients physical health improvement, better emotional well-being and personal empowerment. These assessments lead to more accurate diagnoses and targeted interventions, which can significantly improve treatment results. Natural and lifestyle-based interventions also reduce reliance on medications, decreasing the risk of side effects or dependency on pharmaceutical treatments.
Relapse is common in addiction recovery, especially when treatment doesn’t address the underlying causes of substance use. By stabilizing the systems that influence cravings, energy and mood, functional medicine can reduce relapse risk. A holistic addiction treatment program also helps patients find their inner calm, gives them a safe space to start their therapy and allows them to gain perspective by connecting with their inner selves. Both models can address short-term stability and long-term healing when traditional recovery meets functional medicine, improving the odds of sustained recovery.
This story was produced by The Sanctuary at Sedona and reviewed and distributed by Stacker.
![]()
