Top health experts caution against reopening society before coronavirus testing capacity expands
States may be planning to reopen businesses and communities despite the continuing coronavirus pandemic, but a group of top public health experts cautioned Tuesday against doing so before testing capacity expands significantly.
The president of Harvard’s Institute of Medicine, Dr. Harvey V. Fineberg, said it’s not a choice between dealing with the disease or dealing with the economy. “We have to do both,” Fineberg told a symposium sponsored by Harvard’s T.H. Chan School of Public Health and the New England Journal of Medicine.
Different parts of the country are in different stages of the epidemic with New York well into the first wave and other places just beginning to see the impact of the disease. This matters, said Caroline Buckee, Harvard associate professor of epidemiology and the associate director of the university’s Center for Communicable Disease Dynamics.
Knowing where the virus is spreading is key to relaxing social distancing and returning to normalcy, Buckee said.
In addition to different parts of the country seeing different disease curves, there are “important epidemiological timelines here where when you become infected you’re spreading the virus, but you don’t show any symptoms for about five days or so,” Buckee said. “For people who end up in the hospital, that takes another week and then disease progression from there to death takes another week or more,” she added.
“So, there’s a long time lag between when people are becoming infected and when we’re starting to see an uptick in deaths. And I think that really highlights the important problem here of lack of test capacity. This has a been a problem from the beginning and it continues to be patchy,” she said.
The lack of testing capacity is a big problem because the disease has “a very broad clinical spread,” Buckee said. So even as people show up at the hospital and get tested, there are many more cases in the community, including mild and asymptomatic cases that go undetected.
“And those are the people that are spreading the disease. Right now, we don’t have good estimates for where we are on the epidemic curve in different places,” said Buckee.
“So discussions of relaxation of physical distance, which do seem to be having an effect, curbing some of the worst impacts of the outbreak, need to be based on the capacity to test people so we know where we are.”
It’s important to learn whether people who have recovered can still spread the disease, noted NEJM editor Dr. Eric Rubin. “What we really need is some epidemiologic data to tell us are people who have left the hospital going on to transmit the disease,” Rubin said. “That’s kind of the shoe leather epidemiology, contact tracing, following what happens to the context of those patients, which takes some manpower.”
Buckee added that without knowing the answers, the nation could reopen too soon and risk a deadly second pandemic wave.
“Right now, we don’t have good estimates for where we are on the epidemic curve in different places. So, discussions of relaxation of physical distance, which do seem to be having an effect, curbing some of the worst impacts of the outbreak, need to be based on the capacity to test people so we know where we are,” she said.
A preprint, or non-peer reviewed study, released Friday found that many more people likely had been infected with Covid-19 in Santa Clara County in California than got official diagnoses — perhaps as many as 50 to 85 times more cases.
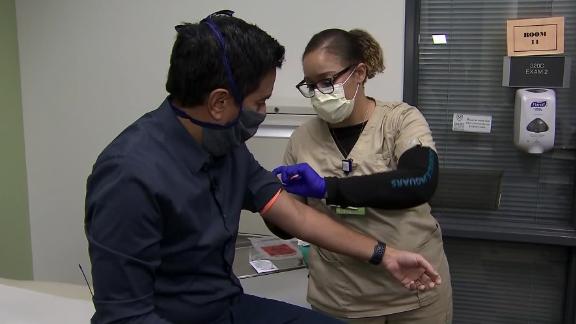
There are two types of tests: one that looks for actively circulating virus and another that tests for antibodies to the virus, an indication a person has been infected at some time in the past.
“Until we know how far along the epidemic curve we are, we can’t really make informed decisions about opening up and how to do that in sensible way because we simply don’t know whether we’re close to the first peak or not,” Buckee said.
“We could see a second wave that could be even more deadly. So really understanding where we are in the epidemic curve, which will be different in different places, is where we’re at. And I think, again, the call for testing is the most important.
The director of the US Centers for Disease Control and Prevention, Dr. Robert Redfield, told The Washington Post that a second coronavirus outbreak could emerge this winter in conjunction with the flu season to make for an even more dire health crisis.
At the White House briefing Tuesday coronavirus task force coordinator Dr. Deborah Birx was asked about Redfield’s comments and emphasized the importance of testing, too.
“We were very clear in the guidelines that we believe we can monitor, again, monitor communities at the community level,” she said.
The Johns Hopkins University has been keeping track of coronavirus statistics and says so far 4,035,860 tests have been performed in the United States, but it’s unclear the exact number of people who have actually been tested as some people have been repeatedly tested for the virus and others just once.
The CDC’s own guidelines warn against reopening communities until certain criteria have been met including making sure disease transmission is under control and that health systems are able to “detect, test, isolate and treat every case and trace every contact.”
