Does your heart beat faster when you stand or sit up? Learn the symptoms of postural orthostatic tachycardia syndrome

GaudiLab // Shutterstock
Does your heart beat faster when you stand or sit up? Learn the symptoms of postural orthostatic tachycardia syndrome
woman leans on couch trying to stand up
If you’re new to the world of POTS, whether that’s because of its newfound connections with Long COVID-19, or its recent momentum on social media, you’ve probably come across the long list of symptoms that may or may not mean you have it.
POTS stands for postural orthostatic tachycardia syndrome and shows up through symptoms like a rapid heart rate after standing, lightheadedness, or fatigue. If you, like many others, have been experiencing this odd collection of symptoms, it’s worth asking the question, “Do I have POTS or is it something else?”
To answer this, Guava Health compiled a list of common symptoms that occur in POTS patients. A few conditions that might mimic or resemble POTS and the key factors that distinguish them have also been highlighted.
What is POTS?
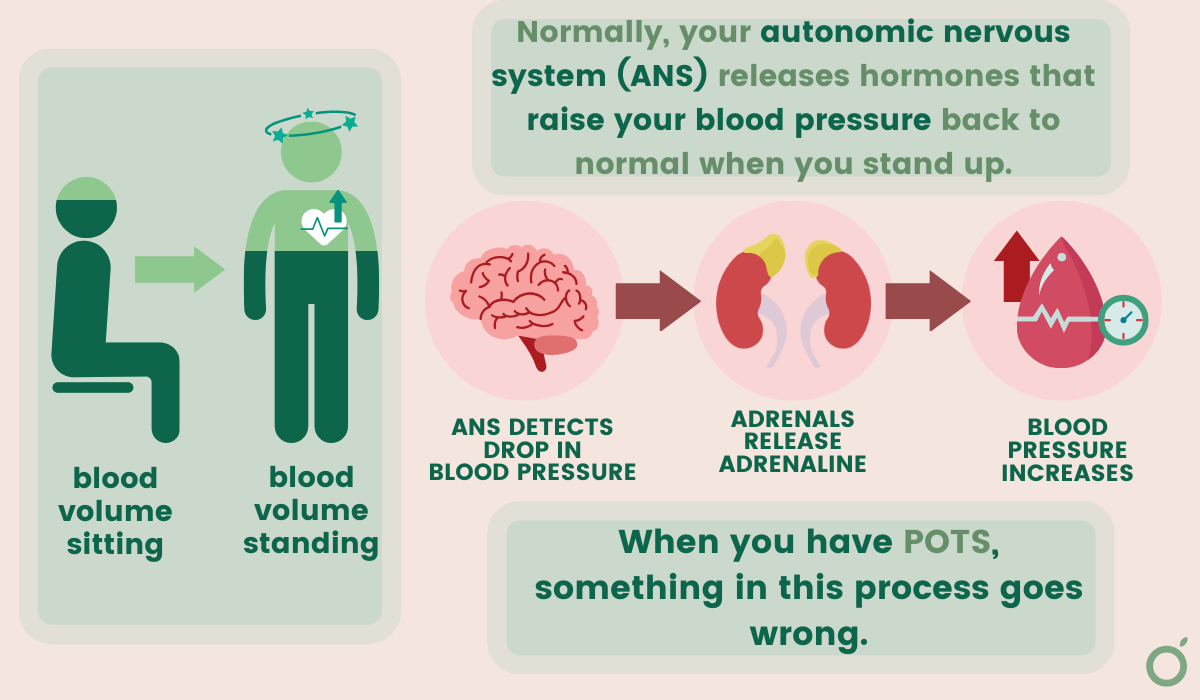
POTS, or postural orthostatic tachycardia syndrome is characterized by an abnormal spike in heart rate when you stand or sit up. It has to do with dysfunction of the autonomic nervous system, which controls a few of your bodily functions that occur unconsciously, like heart rate, blood pressure, breathing, and digestion. This is why you might also hear POTS referred to as a type of dysautonomia, or autonomic nervous system dysfunction.
The most common symptoms of POTS are rapid heart rate within 10 minutes of standing or sitting up, lightheadedness and fainting, fatigue, brain fog, nausea, and shortness of breath.
It’s worth noting that it’s normal for your heart rate to speed up when you stand. What makes POTS abnormal is the timing and duration of symptoms.
To better understand it, let’s break down some of the jargon:
Postural is a word used to talk about body position, specifically standing up or sitting up versus lying down.
Orthostatic specifically refers to an upright posture.
Tachycardia describes an abnormally rapid heart rate.
By stringing these words together, you can see that POTS is a description of symptoms that commonly occur together, otherwise known as a syndrome (that’s what the “S” stands for). Syndromes are different from diseases, which usually have defined causes and effects. Although researchers learn more every day, the symptoms that define POTS seem to be caused by a multitude of factors, making it harder to pinpoint and treat.
Getting a POTS diagnosis is no simple task — the average time it took to get a diagnosis was about 5 years in 2019. However, with the advent of online chronic illness communities and access to health information, that timeline may be shortened.
What causes POTS symptoms?
POTS symptoms can be caused by several things, but the underlying issue is that POTS patients’ bodies have a harder time pushing blood back up toward their heart and brain after sitting or lying down for too long.
When you’ve been lying or sitting down for a while, gravity causes blood to pool in your legs and feet. Your body normally compensates for this by constricting blood vessels and increasing heart rate to maintain blood flow to the brain and other vital organs.
In POTS patients, this pathway doesn’t work quite right. Some people simply have low blood volume, so there’s not enough blood to push up in the first place. Others have issues with their autonomic nervous system, with too much sympathetic (fight or flight) response and too little parasympathetic (rest and digest) response.
All of these mechanisms make POTS patients’ hearts work harder to cause the same response: increased heart rate after a few minutes of standing and not enough blood flow to the brain. These factors are what add to the unique cocktail of symptoms known as POTS, including lightheadedness, brain fog, shortness of breath, etc.
![]()
Guava Health
Conditions that may mimic POTS
graphic showing what goes wrong in POTS
Because POTS is such a complex condition, the line can be a bit blurry between a co-occurring condition and an alternative diagnosis. There are tons of conditions that have the same symptoms, but there are also certain conditions that we know occur more often in POTS patients than others. A few of these conditions are explained below.
Iron deficiency anemia
Like POTS, iron deficiency anemia can cause:
- Fatigue
- Shortness of breath
- Heart palpitations
- Headaches
Iron plays a huge role in helping your red blood cells deliver oxygen to your brain and body. When you don’t have enough iron, whether it’s because of nutrition, genetics, medications, or menstruation, it causes a lot of the same responses as POTS.
Although symptoms of low iron can mimic POTS, there’s also evidence that low iron and POTS sometimes occur together. A small pediatric study from 2013 found that 25% of teenage girls with POTS also have an iron deficiency, whereas only 9% of teenage girls in the general population have an iron deficiency.
Low blood pressure
Although there are key differences between having POTS and low blood pressure, there is some significant overlap between the two conditions. Their common shared symptoms are:
- Lightheadedness or dizziness
- Nausea
- Fainting
- Fatigue
- Heart palpitations
- Headaches
Despite these similarities, a POTS diagnosis requires that patients don’t normally experience low blood pressure. Nonetheless, each patient is different – some people may experience changes in blood pressure with POTS, whereas others don’t.
The key difference between the two conditions is the increase in heart rate upon standing. If you have low blood pressure, this shouldn’t occur regularly.
Thyroid dysfunction
Your thyroid gland releases thyroid stimulating hormone, which is a super important regulator of metabolism and other bodily functions. Dysfunction of your thyroid gland can happen in a couple of ways: hyperthyroidism (when your thyroid gland is overactive) or hypothyroidism (when it’s underactive).
Hyperthyroidism makes your metabolism go too fast, which can speed up your heart rate and cause feelings similar to anxiety, which is why it could be mistaken for POTS.
Alternatively, hypothyroidism does the opposite and slows down your metabolism, which, like POTS, can cause fatigue.
The symptoms that make thyroid disorders different from POTS stem from metabolic issues, too. However, instead of heart rate jumps or fatigue, there are often weight changes, cold or heat intolerance, and changes in hair or skin.
Anxiety
Anxiety and POTS have a somewhat complicated relationship. This is mainly because they have lots of overlapping physical symptoms, like rapid heart rate, dizziness, fatigue, and brain fog, which can make it hard to tell the difference between the two.
A study performed in 2018 indicates that even though people with POTS might seem more anxious, their anxiety tends to be more about their concern over their physical symptoms, not the kind of anxiety seen in anxiety disorders. That’s to say that while POTS patients might be more sensitive to how their body feels, this doesn’t always mean they have an anxiety disorder.
It’s recently come to light that women are more likely than men to be told their illness is “all in their head.“
Despite this statistic, the women in this study didn’t even show a significantly higher rate of psychological disorders. Women’s symptoms are often downplayed or misunderstood, which only widens the gender gap between diagnostic delay and the effectiveness of treatment. This article explains more about the relationship between gender bias, anxiety, and chronic illness.
Guava Health
Other conditions associated with POTS
graphic explaining ehlers danlos syndrome
Since POTS can be caused by so many different factors, it’s common for those same factors to be related to other conditions too. Here are some conditions that frequently occur alongside POTS, otherwise known as comorbidities.
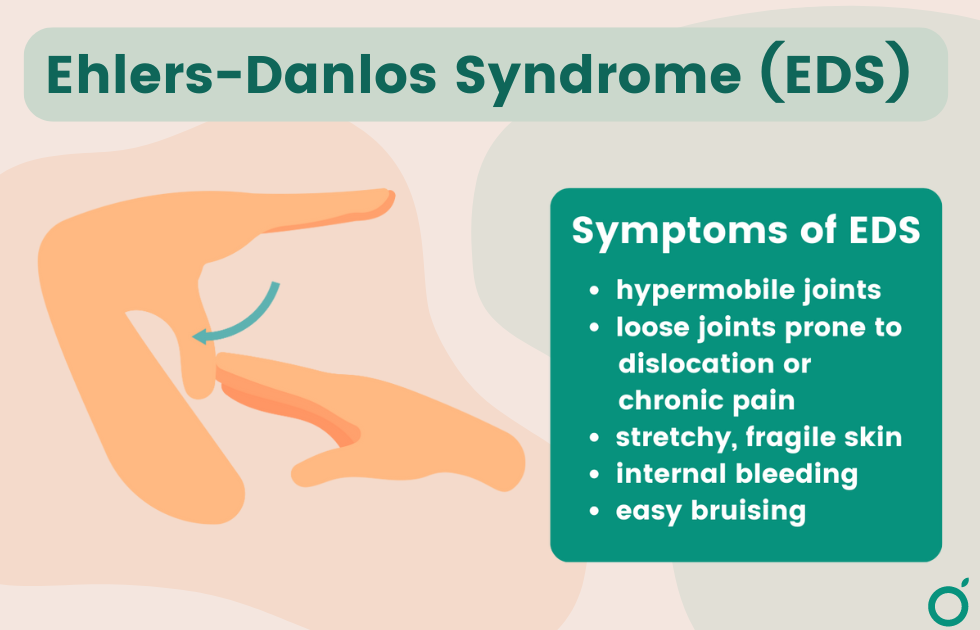
Connective tissue disorders and POTS
Connective tissue disorders, like hypermobility spectrum disorders (HSD) and Ehlers-Danlos syndrome (EDS), share many of the same symptoms as POTS. There’s compelling evidence that besides co-occurring, connective tissue disorders can sometimes cause POTS as well.
A hypermobility spectrum disorder describes the over-flexibility of connective tissues throughout the body. Ehlers-Danlos Syndrome falls under the umbrella of hypermobility spectrum disorders.
When connective tissue isn’t strong enough, it can cause symptoms such as:
- Over-flexible joints
- Fatigue
- Dizziness
- Digestive issues
- Headaches
If you want to know more about why Ehlers-Danlos syndrome and POTS often go hand-in-hand, this article takes a closer look.
Long COVID and POTS
“Long COVID” is the umbrella term for the numerous conditions and symptoms that tend to occur in patients four or more weeks after a COVID-19 infection. Ever since its recognition by the medical world, doctors’ offices are seeing more and more women getting POTS following COVID. Of their mostly female sample group, 66% of patients displayed moderate to severe autonomic dysfunction, which is known as one of the root causes of POTS.
The symptoms of Long COVID tend to mirror POTS because of prolonged fatigue, brain fog, dizziness, and rapid heart rate, among others.
POTS is also commonly associated with (but not limited to):
- MCAS, or Mast Cell Activation Syndrome
- Small fiber neuropathy
- Chronic fatigue
- Migraines
- Post-concussive syndrome
- Electrolyte imbalances
How to differentiate between POTS and similar conditions
Differentiating POTS from similar conditions presents a unique set of challenges, particularly due to its complex nature and symptom overlap with other disorders. However, there are a few key characteristics that separate POTS from the rest:
- POTS disproportionately affects women from the ages of 15-50, occurring five times more often in females than males. Scientists are still unsure why this is the case, so it’s an area of active research.
- POTS patients experience an increase in heart rate within a few minutes of standing or sitting up. This makes it different from other conditions that generally cause a fast heart rate.
- The onset of POTS can sometimes begin after other major health events, like pregnancy, surgery, or viral illness.
- After its onset, POTS symptoms don’t usually evolve, meaning that your symptoms should stay somewhat consistent between episodes.
- Certain medications may also be triggering POTS-like symptoms. Check with your healthcare provider if you’re curious about the potential side effects of current meds.
Despite all the complexity wound up in POTS, there’s an expanding world of online communities and research centered around diagnosis and management. Learning about patient advocacy is vital in taking control of your health, so don’t be afraid to go to your provider with questions about your symptoms.
This story was produced by Guava Health and reviewed and distributed by Stacker Media.